Jackie Collins, Erin Brokovitch and Parasite Cleanses
/I did something today which caught me unawares, but helps illustrate my state of mind at the moment. We are at that annoying time of the year. It is not summer and it is not winter. Some days are nippy and wet and others warm and muggy, but cold in the morning so getting dressed is a complicated affair. Travelling into work from Brighton I have to get a train to London Bridge and then walk a good 20 minutes across Tower Bridge to my office. The change in weather from getting up relatively early, to reaching my office can be like traversing 4 seasons in one stretch on some days. If I am not equipped for all eventualities I can be either over dressed, under dressed, whipped by the wind and rain with no protection at all or sweaty heaving around an unnecessary rain coat and umbrella. My drawers at home still have predominantly summer clothes but I have to seek out warmer items when the temperature drops. Today I was cursing my trouser drawer which is bulging and yet I can’t find hardly anything to wear. Not because of the vagaries of the weather (although this does feature) but because I have shrunk and my trousers, winter and summer, all fall off me and I look scrappy and disheveled if I wear them. They simply hang off. In the summer I did not wear trousers much so it has been as the weather has begun changing that my trouser problem has felt more acute. Ella found a couple of old pairs of her trousers so I do now have a pair to wear. But this leaves all my existing trousers taking up lots of room with almost no prospect of being worn. Yet. And that was my strange moment. I was musing as I stared at these useless garments. I should just throw them all away. Since being diagnosed there has been quite a bit of clearing out. It is all stuff and what good will it do you if you are not around? What good does it do you now? And I am a person with a lot of stuff. But today my first thought was, just throw them away. And then I hesitated. Would I ever need them? To need them I would have to have put on some weight. To have put on some weight would require time. To put on that amount of weight would probably need quite a bit of time. Dilemma. Do I put them in the charity bag? Might I need them again? That is when I realised I had subconsciously thought about a time in the mid term future when I would still be around. I actually had a thought about me in the future without any ifs or buts, my musing was not about if I would be around but if I would put on the weight I have lost in any time that would justify keeping the trousers.
I
This moment reflects a slow but solid change in how I am experiencing my cancer and what I am thinking about it and its chances of it curtailing my future. I have charted my progression from simple acceptance of chemotherapy as the mainstay treatment for me now and in the future to the seismic changes I have made to almost every part of my life (at least how I look after my self) and growing faith in an approach that sees cancer as something that can be healed. I realised today that for a while I have had parallel emotions, the over riding conviction that I can influence the quality and length of my life, with a shadow that pokes its head and rudely disturbs me at vulnerable times, in waiting rooms waiting for results or when I am tired. This shadow is the Golom that whispers ‘its all rubbish, give in, you know what will happen in the end you are just deluding yourself and possibly everyone else’. So lurch from a unshakeable belief that I can and will beat it (that is what I felt for most of last week) to this to crippling fear, usually precipitated by a twinge in my side, which does happen or a story in the paper. Jackie Collins is the most recent such story. I read in the Sunday papers she has died from breast cancer. She did not tell her family she was diagnosed with stage 4, seven years ago. I was rather impressed - what a lot of noise I have made! I was also quite impressed she lasted 7 years. That would be good. But she was 70. She had 26 years on me before this diagnosis. I am sure at the time she felt cheated of her old age. Oh to get to 70.
But for the most part I am positive and these moments of fear do not last long. When they visit me I read and re read stories of survivors and books by practitioners who believe we can heal and that cancer is not a disease but a symptom. Why would our bodies create something to kill us? Our bodies have been carefully constructed to live. In order to address the cancer I have to address the cause, which is what I have been doing, and help my body wrestle back control. I have probably said this before but I will say it again - imagine if over the past 50 years the medical establishment and pharmaceutical colleagues have, with the best intentions, been using an approach to tackling cancer which destroys the very part of us which we need to fight it, our immune system. The implications are huge.
The more I read and the more I learn of advances in immunotherapies and other alternative approaches, the more this possibility seems real. There are a good number of studies which capture the very poor performance of chemotherapy as a means of extending life. There are a good many studies which expose the death and disabilities which are so often the consequence of it. And yet somehow it remains the mainstay treatment and culturally we have been so accepting we are relieved when we hear a loved one, newly diagnosed, has begun treatment. This is exactly what I did first time. I chose to have chemotherapy as I felt this was ‘belts and braces’ as my oncologist called it - everything I could do to prevent its return. No mother could do less but take whatever measures necessary to live. It is inconceivable to most of us us that not having chemotherapy might in fact give us a better quality and prolonged life. But that is what some studies suggest. Why then is it that for so many of us, chemotherapy feels the only path we can take.
I have been imagining the script of a future blockbuster. Set sometime in the future it would be in the genre of an expose of the tobacco industry or Julia Roberts playing Erin Brokovitch - charting the case against chemotherapy.
This blockbuster would have scenes with a roving camera capturing company directors called into emergency meetings following the publication two new studies - yet another concluding that, bar a couple of relatively rare cancers, additional survival among patients who have chemotherapy is almost nothing above that of those who do not have chemotherapy. The other presents data comparing quality of life among those on chemotherapy and those not on it. The results for those on chemotherapy are shocking, the side effects and related medication and hospitalisation following complications contrast starkly with those on alternative treatments or no specific medical treatment. (This evidence actually already exists). The experience many years before within the tobacco industry overshadows the thoughts of all present. They must be careful that there are no leaks as they begin to consider the implications. What would happen to their business model if this evidence became more mainstream and patients started voting with their feet? What would happen if the families of patients who die from side effects start asking questions?
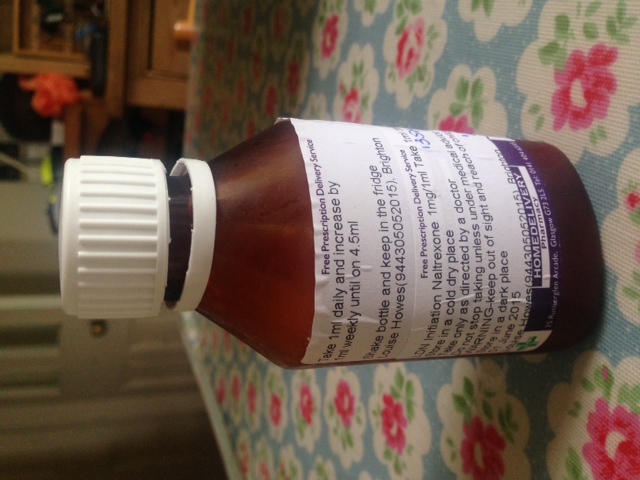
The parallel story in this blockbuster would be that of the protagonist, a handsome relatively junior oncologist who gets to a point where he (or she) can no longer ethically prescribe chemotherapy but has nothing else up his sleeve. Could he really suggest dietary changes? Parasite blitzes? Strategies to destress? Some basic food based supplements (tumeric, fish oils), some vitamin and mineral supplementation and some low cost old drugs (aspirin, low dose naltroxate, metformin). Then would he be an oncologist?
The end of the film would be set at some point in the future when these new targeted therapies and successful immuno therapies are widely available and cancer is more like HIV is today. A chronic disease which can be kept under control in most cases. The period we are living in now would be the last decade of ignorance. Those of us, like the protagonist oncologist in the film, joining the growing global community, connected now by the internet, sharing stories of survival and strategies to heal which do not involve chemotherapy. Picture an underground network sharing healing strategies, working to expose the truth against the odds. Big pharma and their networks stretching through the boards of big cancer charities and health oversight committees, with vested interests - the last thing any of them want to see would be any revelation that might undermine the golden goose of chemotherapy until they have something else up their sleeve to replace it with. So they undermine those practitioners who dare challenge the status quo. Only those drugs and approaches which have undergone rigorous randomised controlled trials can ever be prescribed, anything else ‘has not enough research evidence to support its use’. And so treatments of no commercial value cannot and do not attract the significant investment needed for those special trials. The cost of the trials become a barrier to progress - only those therapies that will make someone lots of money having any hope of getting through this obstacle course.
The protagonist at last is proved right and the community of survivors who took their care into their own hands and rejected convention treatment finally win out. A cultural shift occurs and what was once part of the fabric of the health system becomes a horror story from the bad old days. Children will say ‘when my grandmother was alive she had medicine which made all her hair fall out’.
It would be gripping!
We need more investment in alternative approaches, comparing them fairly to standard approaches today. I honestly could not say that I would never have chemotherapy again. I do not want to. Were I able to join trials that tested new targeted approaches which did not destroy my immune system if my cancer progresses then I would. But for me I have a ladder of treatments ahead which are mainly chemotherapies and hormone if I follow the normal path of someone with advanced cancer. I still believe I am not eligible to go on most trials until I have exhausted known treatments (most chemotherapies and homone treatments). Really?
What is the practical alternative in this period in history where scientific advancements in how cancer works is revealing all sorts of possible approaches to keep it in check, but with these still largely unavailable to oncologists they have mainly chemotherapy, surgery and radiation as their approaches. Healing is imprecise. There is no one pill or drug you caninject. You rely on compliance of the patient to stick to a range of strategies to support the healing process. Not something realistically I can see oncologists around the world ever investing in. It would be much easier to by pass the long intense time consuming healing strategies and give patients a clever drug to outsmart the cancer. Such a drug would be ideal - but it does not exist yet. So in the meantime what do we advanced cancer patients do? We learn not to be afraid. To see cancer as cells that need some attention and a body that needs some repairing. We explore other approaches to healing that those who have survived have implemented and we take charge and simply so no. No I am not going to die. Will to live is the ninth strategy outlined in one of my favourite books ‘Radical Remissions’. If our brains can think we are on an amazing new treatment and respond accordingly even if we are in fact on the placebo then why can't the opposite be true. If doctors more or less tell you you are going to die or there is no cure then might you not simply live out their prediction. So just say no. I am not going to die thank you very much. And that is pretty much the most important first step.
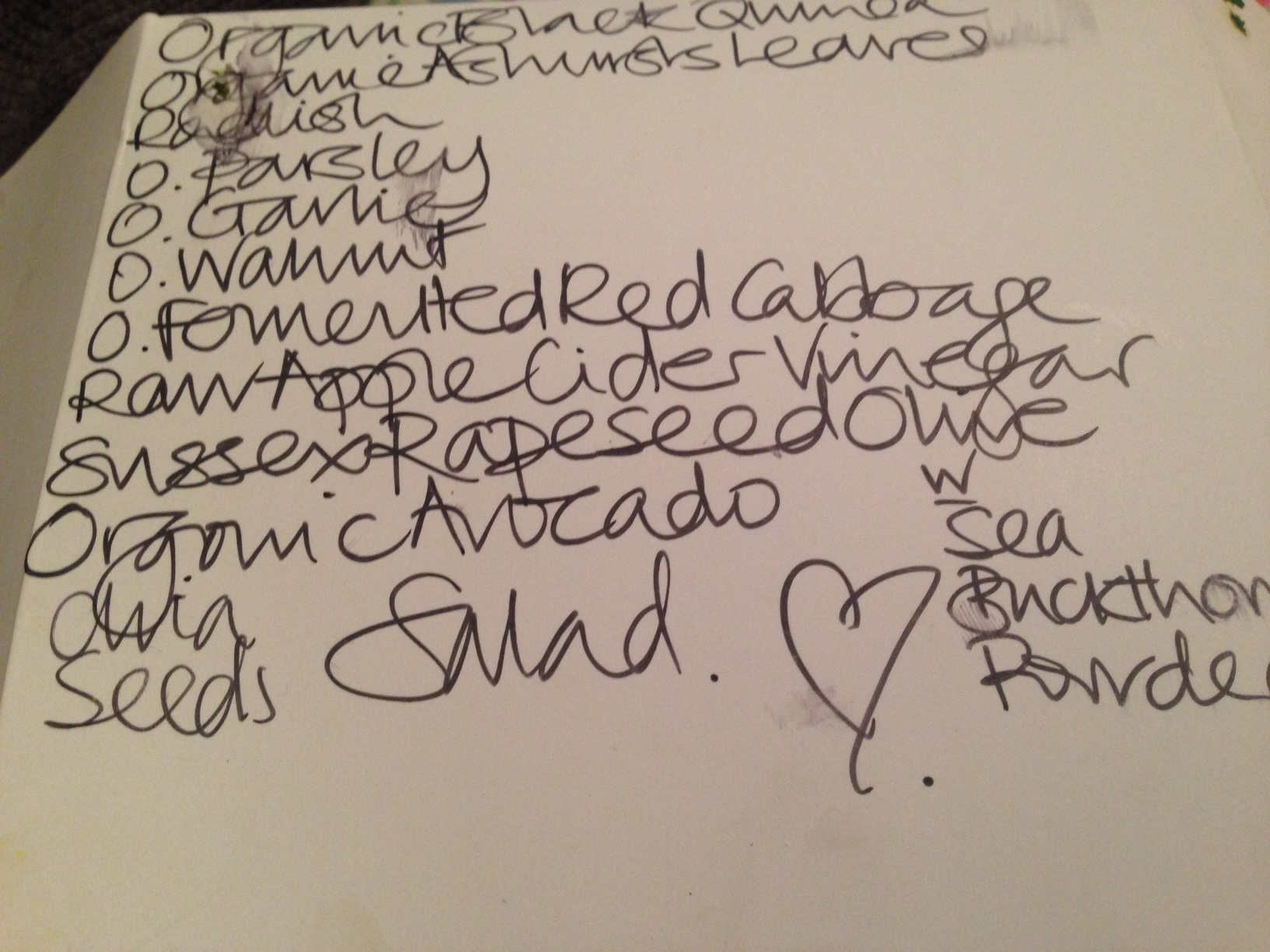
Apart from creating a story line for a future blockbuster I have been getting used to life without Ella. We took her and her bags by train to her University accommodation in London two weeks ago almost. I have seen her twice since then which is probably cheating, but we miss each other. She wrote a long list of instructions for her brothers and Tom has now taken over checking if I am up to date with my supplements and green tea, apricot kernels etc and they all pay attention to my diet in case I am caught nibbling on something I should really avoid. I think it makes them feel they are actively involved in making sure I am well. They are actively involved in making sure I am well.
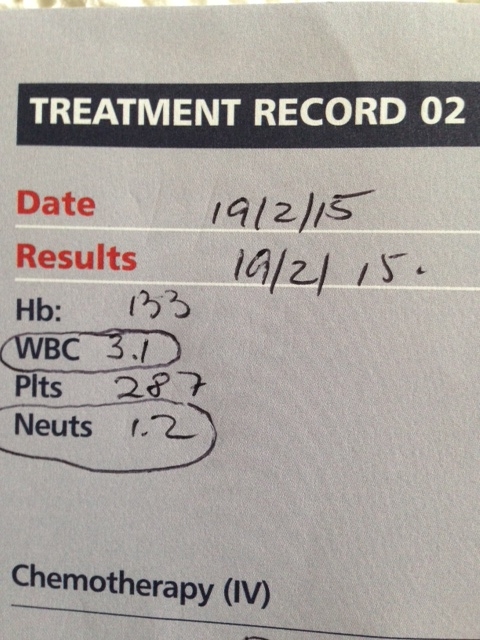
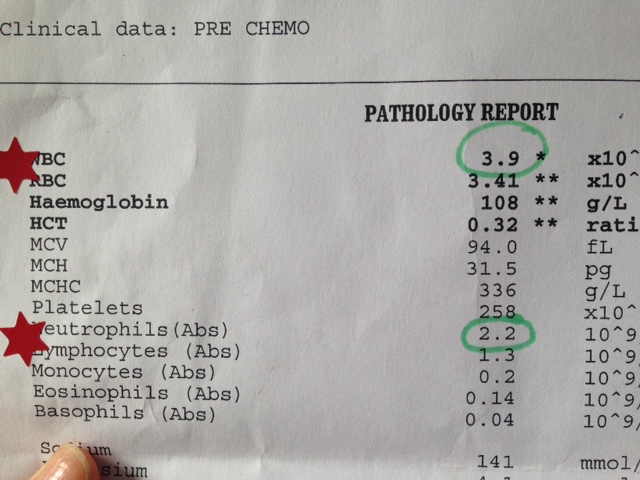
I have also started a parasite cleanse and am exploring how I can increase my juicing, which is time consuming and as a result I do not have enough of them a day. I have been talking to the Juice Revolution the juicing business that works out of the front of Brighton Station. www.jointhejuicerevolution.today. They are passionate about juicing and we are cooking up a plan to try out a way to help me get the vegetables I need, in the right mix, packaged up to make the process easier. I will write more about both next time.
PS Check out this
The shameful past
The history of the discovery of the cigarette–lung cancer link: evidentiary traditions, corporate denial, global toll
Correspondence to
Dr Robert N Proctor, History Department, Stanford University, Stanford, California 94305, USA; rproctor@stanford.edu
Received 5 July 2011
Accepted 22 November 2011
Abstract
Lung cancer was once a very rare disease, so rare that doctors took special notice when confronted with a case, thinking it a once-in-a-lifetime oddity. Mechanisation and mass marketing towards the end of the 19th century popularised the cigarette habit, however, causing a global lung cancer epidemic. Cigarettes were recognised as the cause of the epidemic in the 1940s and 1950s, with the confluence of studies from epidemiology, animal experiments, cellular pathology and chemical analytics. Cigarette manufacturers disputed this evidence, as part of an orchestrated conspiracy to salvage cigarette sales. Propagandising the public proved successful, judging from secret tobacco industry measurements of the impact of denialist propaganda. As late as 1960 only one-third of all US doctors believed that the case against cigarettes had been established. The cigarette is the deadliest artefact in the history of human civilisation. Cigarettes cause about 1 lung cancer death per 3 or 4 million smoked, which explains why the scale of the epidemic is so large today. Cigarettes cause about 1.5 million deaths from lung cancer per year, a number that will rise to nearly 2 million per year by the 2020s or 2030s, even if consumption rates decline in the interim. Part of the ease of cigarette manufacturing stems from the ubiquity of high-speed cigarette making machines, which crank out 20 000 cigarettes per min. Cigarette makers make about a penny in profit for every cigarette sold, which means that the value of a life to a cigarette maker is about US$10 000.
Tob Control 2012;21:87-91 doi:10.1136/tobaccocontrol-2011-050338