At Sea….hot flushes, night sweats and memory issues
/I know that none of this is going to be easy and that there will be ups and down but that does not make the downs any better. I have become an obsessive reader of self-help books - anything with the following in the title will do; how to heal yourself; mind and spirit over body; radical remissions; remarkable recoveries; I healed myself; 12 natural cancer cures; cancer survivors bible and so on and so on. When something rocks me I retreat to my bed (or for an Epsom bath) and practice my breathing while I read one of the above to pull myself together and feed me uplifting content to refocus my brain. This is what I did after the scan. The scan was disappointing. But I was more together after this result than I was the last time I had exactly the same result.
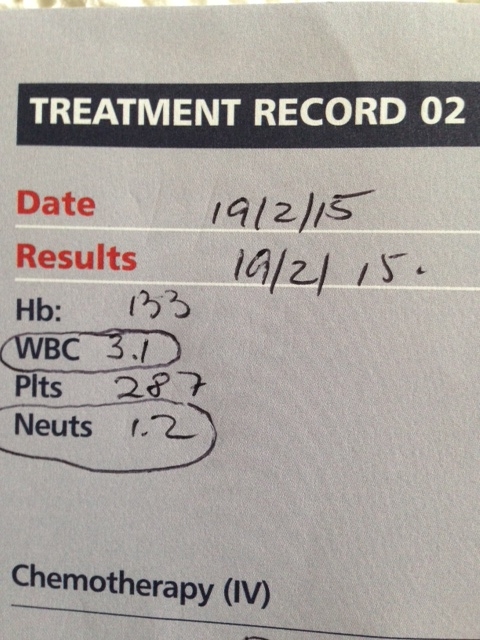
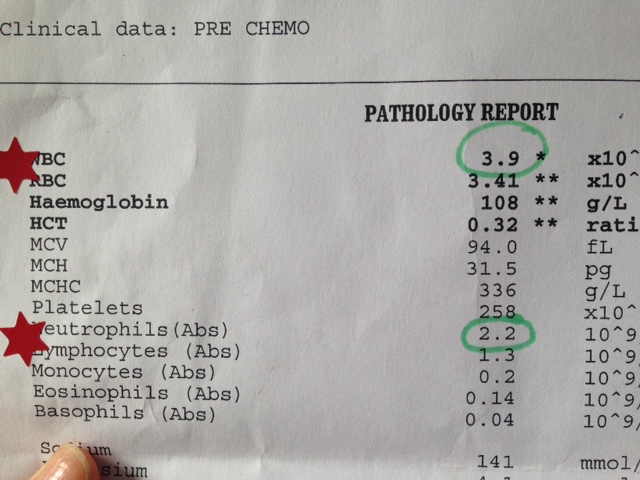
I (with the help of these books and the youtube survivor testimonials) remind myself that healing takes a while – it will not happen overnight. My bloods are good and I am well and this is what matters and my treatment continues. I did want to avoid military euphemisms but sometimes it cannot be helped. The attack continues to get these rogue cells back in order.
I do feel at sea since the chemotherapy, imagining every tweak in my side is the cancer reigniting, every nauseous feeling a result of a diseased liver. It feels like having Golum (Lord of the Rings) on my shoulder, one minute whispering ‘just stay positive, you are healing, all is well’ and then the next (imagine a Golum voice) ‘nasty cancer, cancer is growing, precious cancer’.
I had a test a few weeks ago called a chemo sensitivity test. This costs £1800 and was possible thanks to support for cancer is pants. It involved a sample of my blood being taken and sent to a laboratory in Greece well known for doing this analysis. I had learnt about it from the Inspire website (for people with advanced breast cancer). Members of this site had referred to it as the Greek Test. I live close to an integrative medical practitioner (Vision of Hope Clinic in Brighton) and he also had suggested I have this. It assesses the responsiveness of my cancer against a range of chemotherapies and also natural products.
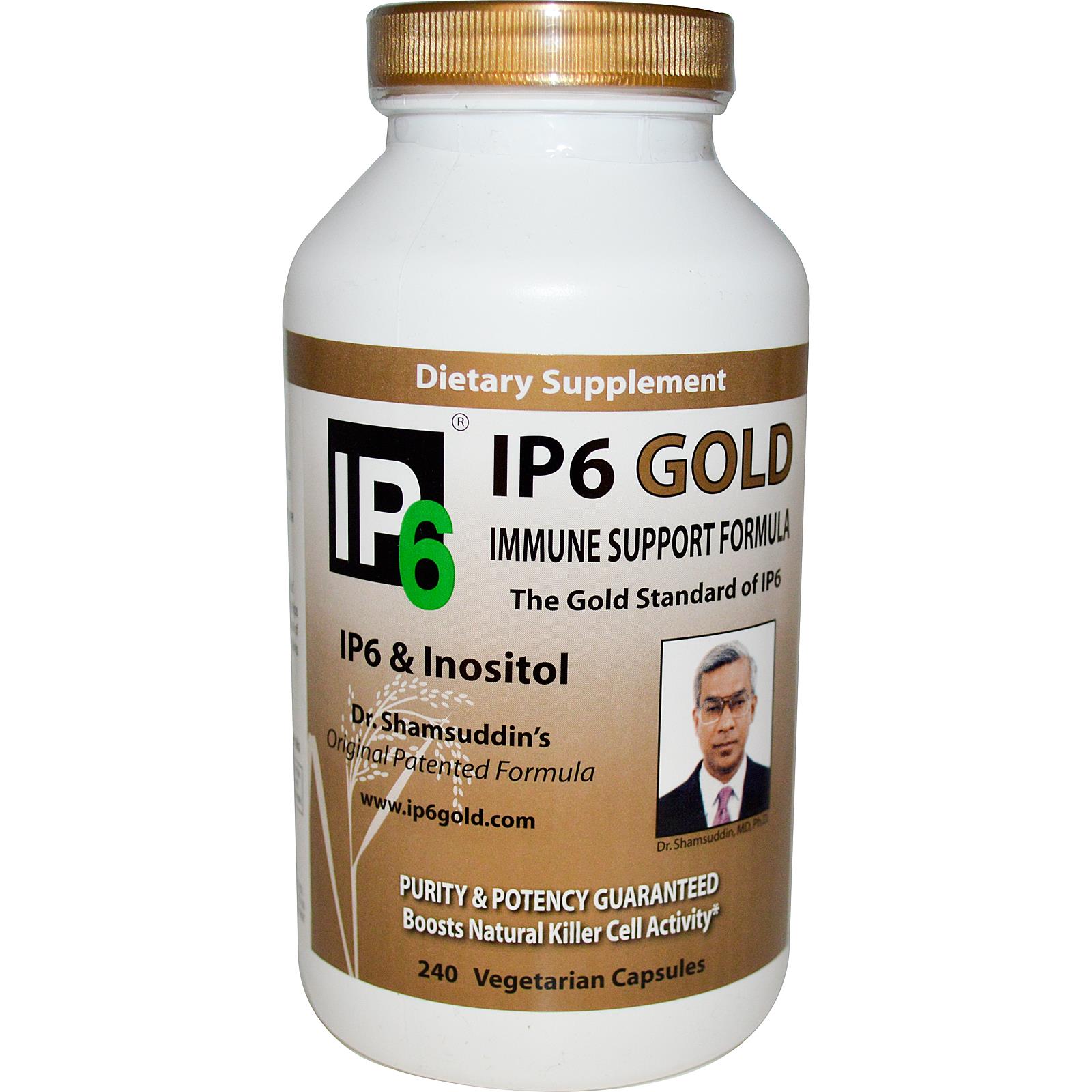
The results came back a few weeks ago and identify about 3 chemotherapies which, according to this analysis, would be most effective on my cancer (in the event I need, or decide to have chemotherapy again). It also indicated responsiveness to hormonal therapies and there were 4 that looked good (including letrozole which I have just started). In terms of other natural supplements I was rather disappointed at how many (or rather how few) supplements looked as if they may influence my cancer directly. This does not mean other supplements will do nothing, they can still work to strengthen my immune system but only a handful looked as if they would actively act on my cancer. These included super artimisinin (which I had started already), paw paw (I had to work out how to source this), and B17 (or apricot kernels). So I have updated my supplement regime to reflect this.
A bit more on chemosensitivity tests
Cancer doctors principally rely on the statistical analysis of large treatment trials, to decide which drugs to use for specific cancers. There is a growing interest, however, in personalised cancer therapy, which involves identifying those treatments which may work best for an individual’s cancer. Chemosensitivity testing is one method of doing this.
Chemosensitivity testing involves testing an individual’s cancer cells in the laboratory to see which drugs demonstrate the best response. It therefore provides guidance about which treatments may be best for the individual in clinical practice.
The test involves a blood test (or sometimes tissue). Tumour cells are identified and isolated from the sample for the following analysis:
• Viability testing of chemotherapy drugs
• Genetic profiling for guidance about targeted therapies eg; monoclonal antibodies
• Viability testing (and identification of mechanisms of action) of natural substances which may be used as part of a complementary treatment strategy .
The results are presented in a written report which your doctor can use to help guide your treatment options and choices.
http://www.rgcc-uk.com/chemosensitivity-testing/
http://www.positivehealth.com/article/cancer/cancer-chemosensitivity-testing
Alongside my supplements my hormone treatment has now begun. As my cancer is estrogen responsive – ie it feeds on oestrogen, hormone treatment involves reducing the amount of oestrogen circulating in my body. The drug that I have been prescribed to do this is called letrozole but it is for post-menopausal women hence the need to put me into menopause via a monthly injection in the first instance. I had this on Friday. I had not really focused on the side effects of this or of letrozole as I had been focusing on the chemotherapy, and then the time was upon me.
I went to my local GP surgery and saw my GP before the nurse who gave me the injection. I used this as an opportunity to politely feedback to the GP practice that they need to get their act together when it comes to ‘non specific symptoms’ from women who have had primary breast cancer. When I first started getting very dry skin and some non specific symptoms like heart burn and I went off alcohol I was treated very slightly as if I was experiencing the ‘very understandable fear factor’ that people who have already had cancer can feel when they get a strange twinge or ache. And it is true, I had lost confidence in my body and every time I got some strange symptom cancer would of course cross my mind. In this instance I went back to the Doctor 3 times in a short space of time. The last one to get a letter for my work insurance company, as I had to cancel a work trip to Zimbabwe and Malawi because of my symptoms. Did this spark anything? The blood test I had prior to this particular appointment had come back with ‘satisfactory’ scrawled on it by the GP who had reviewed it. What I know now but would not have known then, is that despite all the blood data (including for my liver) being fine, they had not tested for the one marker that would have been raised (GGT). In fact the ALT (a marker of inflammation) was in fact just one point above the normal range and the other markers were on the higher end of normal. I persisted and kept going back until I was referred but I wonder what would have happened had I simply accepted that these bloods were good and not persevered until my symptoms really were unbearable and possibly life threatening.
They have been a great GP surgery for myself and my family for many years but I fear this is a chain of events that would have been similar in GPs across the country. Itchy dry skin, tiredness, heartburn would all suggest (among other things)something is up with the liver and therefore if someone with primary breast cancer in the past experiences this, the least the GP should do is really check it out.
As it is, nothing would have changed the fact that the cancer had made a home in my liver and I am where I am. So after my discussion with the GP who prescribed the letrozole and injection I went to the nurse. I had imagined the injection would be a bit like a vaccination but in the fat in my stomach rather than my arm, so I was quite relaxed about it. The nurse, who knows my family and has given all of us injections at some point in the past, tried the get it over fast approach, rather than warn me that it might be uncomfortable (love this euphemism) in case I tense up. As it was it was absolutely excruciating and I was in such shock I burst into tears and asked dramatically if she had accidentally poked it into my stomach or my muscle. The needle was huge with a hole through the middle of it, once it is in your stomach there is a staple like movement which shoots a small rice like pellet subcutaneously which slowly releases hormones to induce menopause. So not only did the injection of the needle hurt, it was followed by an electric staple shock.
I am usually quite a toughy when it comes to needles and procedures, and have spent the last few chemos watching as the nurses have tried various veins until they get one that will work, quite unmoved, so I was surprised my reaction was so dramatic. I think I am just feeling a bit physically vulnerable, I am tired from the chemo and not as strong as I was and I have been prodded and poked quite a bit over the past 16 weeks and this sudden unexpected pain was just enough. I lay there crying for a bit and the pain subsided. I felt bruised but by the end of the day it had settled down. I felt slightly embarrassed at my outburst and asked the nurse if she had ever had anyone else react so badly. She said yes one woman had become hysterical. Which I think makes me her second most dramatic patient.
I then went to pick up the first of what I hope are many supplies of letrozole. Hormone treatment can be as effective as chemotherapy treatment (and in this case I hope it will be more effective) but it can take 2-3 months to kick in. So I do feel slightly at sea. The scan shows the cancer. What is it doing? Sleeping? Inactive – not really sure what that means. I imagine I can feel my liver all the time and have to remind myself to breath and manage this fear. I have a new mantra from one the books I am reading. Breath in calm. Breath out smile. So if you see me walking around with an incongruous smile on my face I may be bringing a fear under control.
Side effects from chemotherapy are one thing, side effects from induced menopause are another and I have a lovely leaflet that lists them all out carefully so I am in no doubt. I need to consider how best I avoid or manage these but here they are:
- Hot flushes
- Night sweats
- Vaginal dryness
- Palpitations
- Mood changes
- Joint pain and risk of osteoporosis
- Bladder problems
- Putting on weight
- Fatigue and tiredness
- Changes to hair and skin
- And the one I find particularly worrying ….effects on memory
Chemotherapy can induce menopause also and while I felt pretty lucid for much of the treatment I have noticed that my brain has a more cotton wool feel to it that it did before. The number of times my children either finish off my sentence or second guess a word I can’t think of is increasing noticeably. Although I have to say they claim my behaviour is no different to pre treatment. At the weekend we went on a walk and I forgot to change my soft shoes for gumboots so, once we hit some mud I had to go back to the car to change them. Once I had changed them I realised I could not find the car keys and spent about 10 minutes searching, on the car seat, in the foot well, under the car. Where could I have put them? Pockets – had none. I was contemplating simply closing the car door and walking back to join Rupert so we could at least continue on the walk. We could search more when we got back. And then as I stood up to close the car door I realised that I had been holding the keys (on their key ring) between my teeth all that time. The leaflet on menopause suggests doing puzzles and crosswords, tasks to keep those brain cells moving. Gulp.
Packing my supplements
And now of course there is Germany. I am nervous to get too excited about any treatment as I need to protect myself from disappointment if it does not do what I hope it will but I do feel hopeful that this team in Germany have good experience at working with people to extend their lives, keep their disease stable and as I have said before, in some cases achieve a full response. In addition to the vaccine I will have hyperthermia to the liver. This involves heating the liver up (cancer is not as robust as healthy cells and does not like heat) with lasers. My chemotherapy sensitivity test indicated that my cancer was vulnerable to heat. Luckily there is still a good deal of cancer visible in my liver for it to get to work on! (that is the Pollyanna response) .
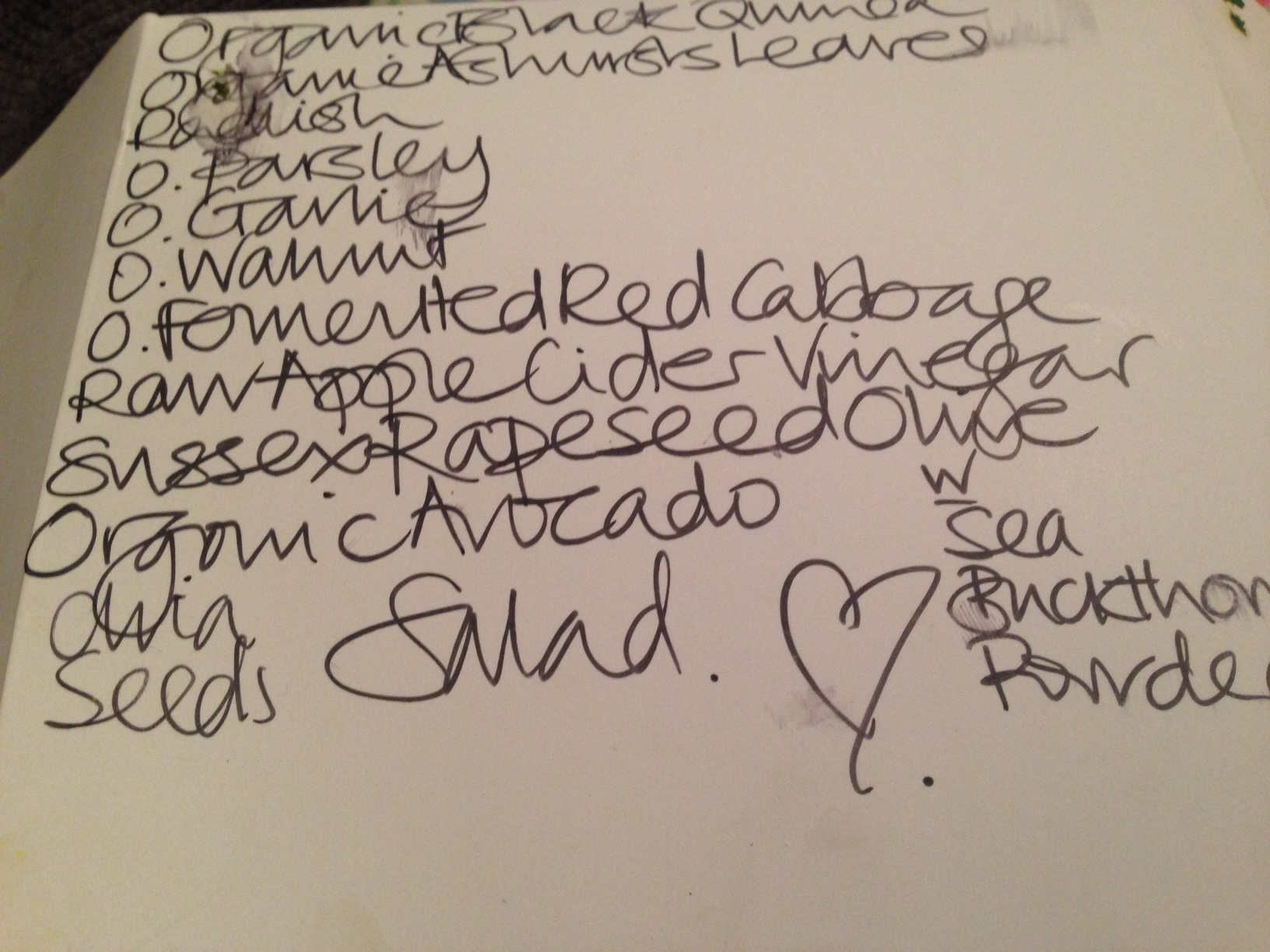
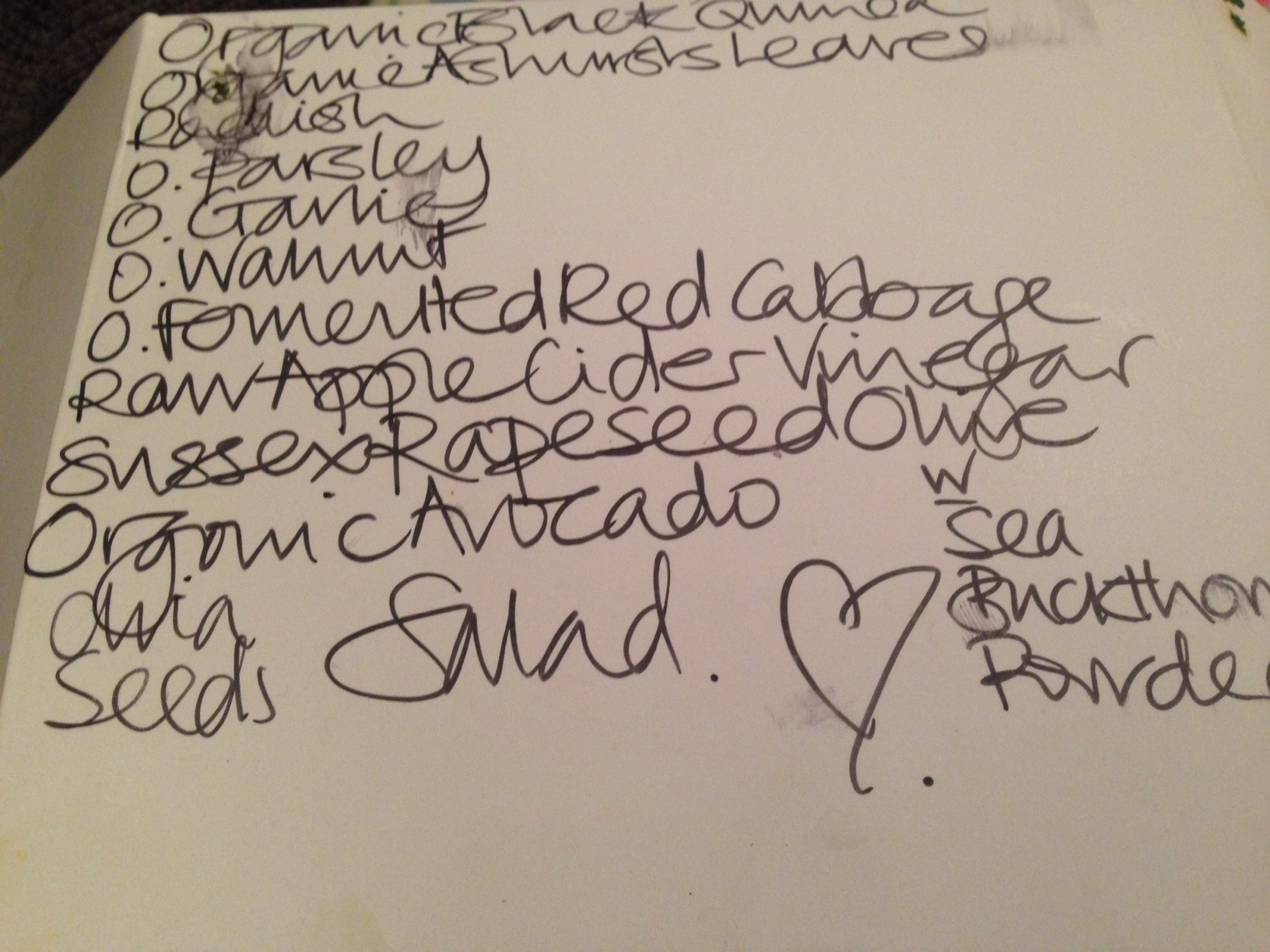
Super foods chia seeds bee polen green tea almond milk sauerkraut and ashtanga powder
Before I go to Germany I have a small mini break to Portugal with my husband. Through all of this Rupert and I have had so little time together. He has continued to work and had taken on a greater load at home and with the children. He has just been on a holiday with the two younger boys, which I would have normally gone on with them during half term but we reckoned it was too soon after treatment. He travels with his job and when he is home we get on with family life, but as I get most tired in the evening he takes on more of the parental role (and when he is away Ella does this). But we have not had any special time together, except a few walks at weekends.
The not-so-compact Juicer!
This is not enough time for us to really talk. We immediately swung into action to absorb and make family life as normal as possible, to communicate that life remains joyful and hopeful. We had to, and continue to go through some administrative must dos in this situation, including scenarios for an unknown future – financially, administratively. Most of the direct debits related to the kids comes from my bank account, their pocket money, telephone deals, the family netflicks account, the apple account etc. We have not worked these out but I have been compiling a list so that we can slowly transfer these to Rupert’s account, just in case. I recently signed Ned up to something which I have to control of until he is 13. Of course I intend to be here when he is 13, that is only next year, but these situations continually arise. A 5 year guarantee for something. The expiry date on my debit card. All reminders.
Anyway, before I even knew I would get to Germany Rupert had a work meeting scheduled for Wednesday to Friday in Portugal so we agreed it would be a good time for me to have a small break after treatment and booked me to join him. The first ever work trip I have ever accompanied him on. This is a 3 day break and I arrive back on the Saturday but leave for Germany the next morning so my bedroom is covered with suitcases and piles of clothes. I have even bought a compact juicer so I can continue juicing (not sure it is quite as compact as I had imagined), and I have organised my supplements into little bags for each day. I have failed so far to purchase a swim hat and am still not quite sure how I manage a) lounging by the pool – my skin is super sensitive to sunlight still, my wig would be super hot and bald would not be a good look. The problem with thin scarves are that if they come loose it is really difficult to adjust them without a mirror b) a walk but along the beach – if there is a sea breeze it will blow the wig up revealing its wigness. Here I wear a beanie hat (even when the sun is out sometimes) to keep it attached . I need to practice with scarves again, but this time ones to keep the wig in place.
Working out administrative and financial arrangements is on-going, working out our emotional response to the possibility of me not being around is something different altogether. We know we have had over 20 amazing years together and have been blessed to have had this time, but suddenly our future, or the range of futures we had imagined, have been blown away. We are working on terminology. I am not ill, I am healing. I am not dying, I am living. Uncertainty is a feature of everyone’s lives, our imagined futures were just that. Nothing has changed. We must now focus on now and everyday. Having some time to work through this together is what we need.
June 3rd - At the airport ready for some Time together.