Reduction in tumour activity; talking cancer and blue legs
/I am back from my second TACE treatment in Frankfurt. This time to my left lobe. Prof. Vogl was decidedly more chatty this time for the few minutes I saw him while lying on my back in my delicious hospital gown. He had looked at the MRI scan that I had a while earlier that morning and reported evidence of reduced tumour load and tumour activity. The latter being more important at this point I understand. This meant he could go ahead with the same cocktail on the left lobe. I will need one more go on each lobe - so two more trips to Frankfurt over the next 2-3 months. But to hear the understated Professor Vogl say he thinks we are ‘on a good path’ makes me feel confident and I was considerably happier having heard his conclusion.
The days before going had been difficult. My left lobe is really quite uncomfortable, it presses on my stomach if I lie in a certain position and I have to prop myself up in bed. It had also affected how I walked which, possibly tension added to the mix, had given me a sore upper back where the muscles are taut. All these complaints seem to have melted away with new hope that things are going in the right direction (except the discomfort in my abdomen which prevents me lying on my front). It is amazing how your mental health so directly affects your physical health. I had a dark cloud hanging over me, worrying that the treatment may not have worked and wondering if this was the case, how many options there would be left given the tumour load was already quite high in the liver. The moment Prof Vogl communicated his conclusions all those worries just fell away. He was happy for me to return in early January which essentially gives me a free pass over Xmas and New Year. A wonderful few weeks to enjoy my family and friends and indulge in being extravagantly Xmassy.
This has involved so far the purchase of a silver wool jumper, putting up the mistletoe lights; buying a small wooden German christmas tree ornament with lots of wooden decorations; making the annual advent calendar (a wooden calendar with doors for each day of advent which I fill with chocolates and sweets); retrieving the gold plastic wreath and hanging it on the front door (sounds tacky and honestly I have usually had holly wreaths but this gold one was quite pretty and I am now reaping the rewards of not having to pay for a wreath this year - felt very pleased with myself); purchasing 2 glass star candle sticks for our kitchen table (using my 20% off Home Sense voucher - which I get on certain days for being the nominated friend or family of Tom who is currently working as a Xmas temp there); buying some Xmas cards in my annual attempt to send my loved ones an actual physical message (usually the first half of my address book receive one, the next few possibly after Xmas and anyone after H is lucky to receive one at all); and the decision to join in the office competition for the best decorated desk space.
Ella came home one weekend recently with agreat friend of hers from Denmark who bought me a present of some make your own decorations. She patiently worked with me for far longer than should have been necessary to teach me how tomake them. My spatial awareness is quite simply hopeless. I did eventually master the heart shaped decoration but the star remains a struggle. My intention is to decorate my desk using my own almost home made decorations - which I reckon ought to win me some points for effort. We have set a date for a Xmas party and I have just bought the Xmas treewhich is usually an entire family affair but with half the family elsewhere - Rupert, Ella and Ned, Tom at work and William at the library as he has mocks next week - I made the choice all by myself for the first time ever. This will I know invite comments about either its height, the level of bushiness and how lopsided it is. I decorated it this evening with Tom and Will. Spotify has various Xmas song playlists and I have begun to listen to these almost on a loop and I have Xmas presents and wrapping paper strewn around the house as I decide to fill odd free moments with a bit of wrapping up, only to be distracted and wander off leaving it slowly taking over any spare space in the house. And then there are the carol concerts I am planning to go to. It all sounds rather desperate but it is in fact rather wonderful. If you think it might all be taken away and then you get it back you hoover it all up - no question. The children have also received their annual advent calendar from my Mother. She now has 15 grandchildren. This is not so much a tradition anymore but an institution. Every year a huge envelope arrives with calendars for the kids. There is a bit of bartering about who gets what - Ella always seems to get the glittery angel or manger scene. This year she accidentally left hers at home so I am enjoying opening it. No holding back. I remember loving it when my calendar from Mum arrived at school. I would get out of bed first thing in the morning, it was always cold, and tiptoe over to it to open the little door. It was a countdown to going home and a to my favourite time of the year.
The tree is now up. And we have had only one incident so far with the dog gobbling a fluffy sheep decoration. Actually I am not sure there was much gobbling involved, mainly just tearing it to almost unrecognisable pieces. I noticed something under the kitchen table and on closer examination realised it was a head. The body itself was strewn beneath the culprit's (Melka) favourite sitting place.
My trip to Vogl this time felt more straight forward. One of my best friends Zoe, who I have worked with for many years, came with me and we basically non stopped talked and laughed. Her task as primary assistant involved, in addition to diverting me with sparking talk, carrying my bags on the way home, be with me through the day of treatment and then helpme take off and put on my trousers, socks and boots after the treatment. This time we worked out that she could come into the operating theatre and watch what was going on. The benefit of having someone else there is they can hear what is said and help you interpret it when it is all over and you want to dissect themeaning to the nth degree. She was sat by the wall with a ring side view and made to wear a heavy lead body protector to prevent gamma rays, or whatever rays the machines Vogl uses give out. This time round the time between being prepared and having the IV line up with anti nausea and painkiller injected in and Prof Vogl arriving was far shorter than last time. Last time I was definitely a bit whoosy and floaty when he arrived and did not really feel any pain just pressure - this time he entered pretty soon and I was still very much alert and not floaty at all. When his big needle appeared I asked in a frantic but pretending to be very together and calm type of voice, if he was going to wait until the painkiller had really taken hold. But he said it would eventually and just carried on. This really was quite painful and I definitely squealed loudly (this time he was going through the femal artery on my left) and he had to inject a good deal more local anaesthetic directly into the area - which left me with a totally numb leg for quite a few hours. One of the main impacts of the procedure is that for a couple of days it is very difficult to lift your leg or put it into certain positions, so I shuffled along the long corridors at Heathrow with Zoe laden down with all our bags as we tried unsuccessfully to flag down a buggy.
This time I had cleverly remembered that as after the procedure it is impossible to wear my relatively tight jeans I needed to pack some soft leggings. Last time, once on the ward under observation, Sophie, who was my assistant number one for that trip, went in search of some cheap leggings so that I would have something to wear when it came to leaving the hospital. She returned with possibly the most ugly blue leggings with plastic dark blue stars splattered over them and elasticated bottoms. It would have been hard to have found anything more unattractive if I had paid her. But I had no choice, knowing that public exposure would be minimal between the hospital, the taxi and the hotel, especially as it was dark by the time we got back to our room. The next day my leg was not better and it was clear that I would have to wear this monstrosity of a piece of clothing to the airport and on the plane. When I arrived home I was very tired.
Rupert had run me a bath and Ella made me my juice. Rupert chatted as I undressed and heaved my leg over the side of the bath ready for a good soak. I looked down and honestly my heart almost stopped. My legs were blue. Panic just welled up - the operation must have gone wrong, maybe the artery was blocked (my biology was never very good). As Rupert updated me on family and work I feigned total calm surreptitiously grabbing my phone which was on a stool nearby and started googling ‘symptom checker, blue legs’. The following medical conditions are some of the possible causes of leg blueness. Vascular insufficiency; coagulopathy; haematoma; peripheral vascular disease; arterial embolus… Or A bluish tinge to the skin is known as cyanosis. It is a very serious sign of low oxygen levels and build up of carbon dioxide’
I felt tired but I didn't feel that bad. My heart just started pumping and pumping and I felt light headed with shock. What was panicking me was not just the dangers of what might be happening physically but more concerning was what this would say about my quest to outsmart my disease and navigate my way through it all. I envisioned myself being rolled into A&E on a trolley; whispers ‘advanced cancer’; lots of well meaning pained faces; ‘tell us the event up to your legs turning blue and what other symptoms do you have’ ‘oh…so you have been to Frankfurt, arrived back today? what were you doing in Frankfurt’ (eye rolls - here we are mopping up after some foreign medical tourism disaster) - I could see the front page of the local Argus ‘woman who’s campaign we supported in mortal danger from complication from treatment in Germany’ - what about all those people who have followed my story and want to know how it goes for themselves or someone they love. I just sat in the bath staring at my legs, grunting acknowledgement in different tones to make out I was listening intently to Rupert, breath shallowing from shock, mind racing - do I call 999 now - perhaps I should rub and get some blood into the legs - stand up and gravity might help. So I stood up and began rubbing furiously. And then a very strange thing happened. The blue started coming off in my hands. And the penny dropped. This was not cyanosis or vascular insufficiency this was staining from disgusting cheap blue german (or possibly Chinese) leggings. Honestly the feeling of relief was almost worth the panic. And then the ridiculousness of the situation which has kept me going for a quite a while - making me chuckle every time I think of it.
Working out what to do next withmy cancer treatment is difficult but I have discovered an amazing woman, who I mentioned before, she is Grace Gawler and has a foundation. She describes herself as a navigator. She has worked helping people with cancer navigate the many options and directions for years and is totally up to date with developments globally. She is connected with some of the most forward thinking oncologists and researchers and has helped me work out what to do given my specific situation. Unlike my oncologist, who is able to offer me only what is available and registered for use in the UK, she can identify potential therapies and advances wherever they are. This is tricky as I have to work any such care in with my oncologist who remains my primary clinician - but it puts him in a difficult situation. Prof Vogl for example simply cannot discuss each individual case with the primary provider. He assesses each patient on whether their clinical condition and treatment profile makes them eligible for treatment and in my case Grace becomes the interface. She helps filter those people who she knows would meet his criteria(I send her my bloods and other information) and then if he accepts you she will help make the first appointment. I pay for Skype sessions with her to talk through my options but also for example my supplements. She has already provided me with information which has made me change some of my supplements. I have stopped coffee enemas during the chemo treatments - as while good for helping with liver toxicity - in this case I actually want to keep the chemo in the liver to do its job. I feel so much more secure having someone with her knowledge helping me work out what to do. As she is not a provider herself she is able to share information, contacts, advise from across the spectrum knowing what my own situation is - geographically, my family, job etc - anything that makes a difference to what decisions I might make. Ultimately I am responsible but I trust her and this has made my job of working out what to do much easier. I was in danger of becoming a fantastically broad generalist with not enough specific knowledge.
I also share ideas with others I have met on line - often with broadly similar disease - and talk about what we have done and are thinking of doing and share information about treatments and advances or problems. The worldwide web really both a dangerous but also incredibly liberating place to connect and build networks impossible just a few years ago. I feel one of a tenacious group of utterly determined individuals who want to stay alive and are in search, as I am, for strategies which might help them do so. Thank goodness I did not die of some blue leg syndrome after my Vogl treatment or this would forever be on the web and deter countless people. That is the danger of the web. There is one blog about someone with advanced cancer, who was in a bad state and sought care from Vogl - it was not successful and he did die. But he also documented in painful detail the treatment and that it did not work and that he was too far gone. I don't know how many times I read this and it did deter me from seeking out Vogl independently. But Grace gave me confidence, she knows his record and he is well published. I could have been ‘British woman with terminal cancer seeks treatment in Germany anddies….Louise Howes of cancerispants fame died tragically after returning home from experimental treatment in Frankfurt this week. The treatment is not currently available in the UK for people with metastatic breast cancer. A spokesperson for the NHS warned patients to avoid being drawn in by claims of extended survival by clinicians offering care that it currently not approved for use in the UK’. But I was not - and anyway it is not experimental at all - but quite established for primary liver cancer and in some places for colorectal cancer metastasised to the liver. I am in no doubt it will not be long before it is made available to breastcancer where the disease is dominant in the liver.
My recent meeting with my oncologist was a bit awkward as he clearly, and unsurprisingly feels that it is difficult for him to safely treat me if I go elsewhere for treatment he is not responsible for. I share details of the treatment. I would really like to be choosing the route I take more collaboratively with him but know that he has to be careful and is to some extent bound by what is approved in the UK - so how can he condone treatments he is not able to refer me to. But he has been supportive. But it is a quandary. I do not believe if I rely solely on treatments available in the UK that I will stay alive as long as I hope I do by taking advantage of treatments that are more targeted that I cannot get here. I know there is a risk involved but there is equally a risk simply working through the current treatments on offer here. So - what to do. Be bold as there is quite a bit as stake - my life no less. I do have a lovely team in the UK who care for me - I think they think I am bit of a trouble maker - polite but not easy to pin down. But one of them recently kindly said ‘I don't think anyone is judging you Louise’ and that made me feel better.
There has been a growing discussion about ‘How to talk Cancer’. There was an article in the New York Times last week and this was shared on the chat boards of Inspire (for people with advanced cancer). I was kind of surprised at the passion this discussion has prompted. I have always felt very strongly that honestly knowing what to say to someone with a cancer diagnosis is pretty hard and I therefore would absolutely not judge anyone for how they approach it, even if this means awkwardness and avoidance. It touches everyone very differently and mirrors peoples own mortality in someway, which make it doubly difficult to talk. Some people find it very easy, often you will find they have known someone close to them who have had or died from cancer and they navigate it more naturally. Others simply do not know what to say and worry that they may put their foot in it. I judge no one. Humour has always been a strategy I have used to get through difficult times and conversations - so I am the first to have rolled around laughing at comments about the savings I would make from not having to pay for hair treatments (honestly it really did save me quite a bit given I used to colour my hair relatively regularly). I don't mind if people talk about the fight or tell me stories of people who overcame it or ran marathons when they were ill etc etc. I know that these people basically want to share their love and be kind - they want to help make it better in someway and that intention is enough for me. So to judge them for the wrong choice of words achieves nothing.
The New York Times piece is about what not to say to a cancer patient. Already I do not like the subject matter. But I kept on reading. It is by a Dr Stan Goldberg a prostate cancer patient and communications specialist at San Francisco University. That says it all already. He is a communication specialist which means he is professionally committed to helping people talk about all sorts of things. So it would make sense that when he got cancer he began studying peoples responses. Goodness i would not like to have been one of those people. How to talk cancer to a communications specialist - you would absolutely put your foot in it. He provides a list of dos and don’ts - already sounds complicated. If you didn't instinctively know what to say you would have to memorise a list of dos and don’ts for fear of messing up - best perhaps to avoid the topic completely and then you definitely wouldn't say the wrong thing.
Among the don’ts were ‘preaching, unsolicited advice or recommendations, judgement and blame, uninvited discussions about prognosis, information about unproven treatmentsand your own feelings of distress’. Well I am sorry Dr Goldberg….I absolutely don't mind preaching, there maybe something useful in it; I welcome all unsolicited advice or recommendations as who knows there may be an amazing nugget in there that could make all the difference; I am not really sure what he means about judgement or blame - perhaps people wondering what may have contributed to me getting cancer - which is actually quite a sensible line of thought, it is not simply bad luck - it is the result of a series of related factors a good few of which would have something to do with my lifestyle or previous medical decisions - in my case probably using immune suppressants for 2 years, eating badly and running round juggling more than should be humanly sensible - all giving cancer a chance to take hold by weakening my immune response - if I do not consider what might have caused it how might I make changes to try and moderate its progression? Then there are uninvited discussions about prognosis. There do exist figures on average survival depending on stage of disease but these are averages and were calculated from data that are already old - so the real answer is actually who knows and I totally understand why people might want to know as it helps them respond. If the answer is that this is a cancer that is very easy to treat and almost everyone survives, that is a good thing and people can feel happy for you and hopeful, it if is that most people do not survive for many years then they are able to respond equally appropriately and be more actively helpful and present - clear about the severity of the situation.
What about ‘information about unproven treatments’ - this is a big one! What on earth constitutes an unproved treatment these days? I have come across many treatments for which there is a good level of evidence of benefit but without the standard of evidence required for it to be accepted as a mainstream treatment. A case of not enough evidence but not unproven. The outcome being these are not being made available to people who may benefit from them. Take metformin - a diabetic drug which helps restore the body’s response to naturally produced insulin and has been shown in many studies to have a protective effect in several cancers - why is this not available to advanced cancer patients? So please talk to me about any sort of treatment that may possibly help - I will then do my research and make a judgement as to the whether it is worth pursuing. And finally talking about my own feelings of distress. Why not? This is the only human thing to do - acknowledge that this must be distressing and have a discussion about it.
But this is my reaction to this list of don’ts. The discussion on Inspire simply illustrates quite how different we all are. Some people felt very strongly about how other people should or should not react and respond. So maybe some advice is useful and necessary.
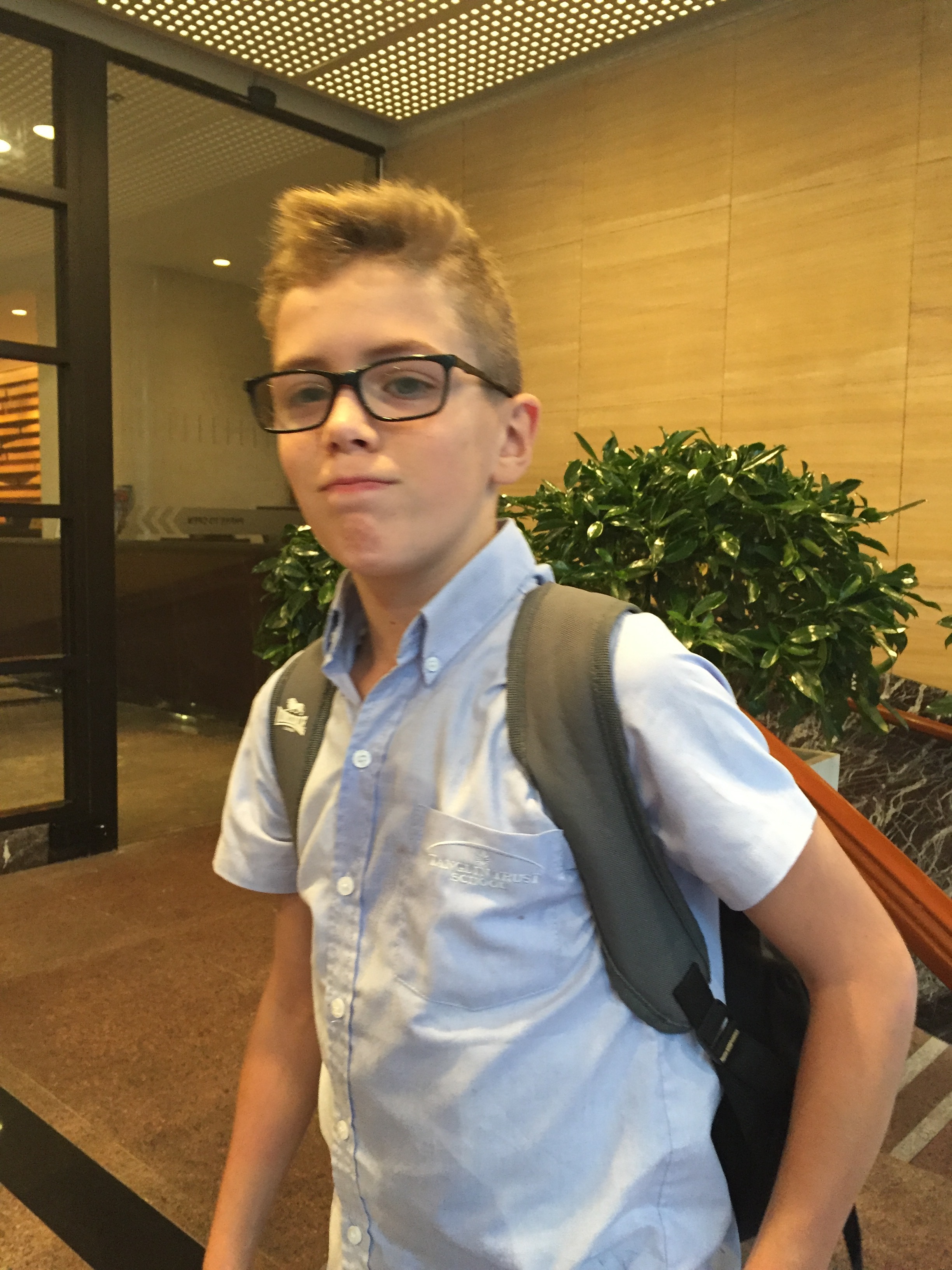
A young man call Julian Quick who has a rare form of bone cancer found that some of his friends and family, and work colleagues were unwilling or unable to speak frankly to him about his condition. He was so frustrated that he started to work on a range of what he calls memes - or illustrations of awkward situations people have found themselves in with advice about how to talk cancer in such situations. He worked with AXA PPP healthcare to help come up with some do’s and don’ts. He found comments about the savings he would make from not having to use of hair products in poor taste, but I think if he spent as much money as I used to at the hair dresser he may well have found these comments less crass. We are all different but there has until now been little advice for either those of us with cancer or those of us who know someone with cancer and these resources begin to fill that gap. They are worth a read and a share.
The other side of the coin is how to talk to people if you are the one with cancer. I am not usually short of words but there are times when it is hard to know what to say, when I am not actually sure what I am feeling or thinking as these are not constants. Having to talk to people a work, strangers or even your nearest and dearest at times. AXA PPP healthcare are about to release/have just released a new guide “Let’s Speak Cancer” as well as a video guide. They are practical and give tips to those with cancer on how to talk about it. I have added the links above but also to the resource section on this site.
In between my work trip to Tanzania and two trips to Germany I managed some very special time away with my husband. He had a work trip that took him to the Maldives (there are worse places to have to go to for work) and so I went with him. We added 3 days on the end of his work trip and it was unforgettable. Our flights went via Singapore so we saw Ned and my sister for a couple of days. If only you could stop time now and then. Or rewind. Let's do that bit again! No - not enjoying this bit - press fast forward. A few pauses here and there would not go amiss.
I made a mad dash to Japan (which I thought was a bit closer to Singapore than it is) as I wanted to visit a clinic which is pioneering a new immunotherapy. Immunotherapy is a term that describes a whole host of approaches and this one is one that Grace Gawler has suggested would be worth investigating. She has referred a number of patients there who are doing very well. So my sister, Cecilia came with me and we spent two nights in Tokyo. I had a consultation and gave blood and some white cells, so they can make up a vaccine for me in the event I decide this is the route to go. It takes 3 weeks to make up the vaccine so when I realised this I thought it would make sense to pay the extra to get there from Singapore so that they have what they need. They have since sent my blood results back. They map the cancer immune system in a very clear way and mine, at the time they took the bloods, does not look very impressive. I seem to be very low in natural killer cells in particular.
I am in no doubt that it will not be long before a cancer patient routinely has their bloods tested not only for signs of progression (e.g. cancer makers) and how the body is coping with treatment (white and red cells etc) but how the immune system is doing to inform oncologists about what the next step could be.
There is also an explosion in the use of genetic mapping - mapping the characteristics of the tumour. I have also decided to have this so we know what treatments might work better to help make decisions about next steps. These are not available on the NHS routinely but you can pay for them and some private insurance companies are approving them. This still means they are out of reach for the majority. If it means it helps us work out how your cancer works and avoids me taking treatments less likely to effective, with all the side effects they bring, then it would be worth it.
This link from Grace describes it in this way:
Genomics-based diagnostic testing looks at changes occurring within an individual patient's tumour to identify options not previously considered. We can now categorise cancer by the underlying gene mutations that drive its growth; instead of naming it by location, e.g. breast, liver, prostate, brain, cancers, etc. With genomic testing doctors have a better chance of finding gene changes causing or associated with your cancer. This information enables doctors to target your cancer in highly effective ways. Tailoring your treatments to your tumours individual characteristics.
I am not sure that our health system is yet ready for this explosion of information - in fact I know that it is not. But one day it may be able to offer genetic testing to all (as happens to most in the USA) and match people with treatments. We still live in a country with the worst cancer survival in Europe and the tragic loss of AA Gill before the publication of his article in the Sunday Times magazine today highlights the lack of access to new drugs within the NHS. He had a type of lung cancer which had particularly good response rates to an immunotherapy called nivolumab. In the USA and much of Europe, and within the private sector here this would have been his first line treatment. On the NHS it was not available to him. Nivolumab may not have saved his life but he may have had a very good chance of more precious time with his family. As the rest of the world steps up to the revolution in cancer therapies those of us with advanced cancers have little choice but to keep up with research on new treatments and do what it takes to access them when the evidence suggests they are likely to give you the best chance at success.